
 Corns are small, circular, thickened areas of skin on the feet that have a central core of hard material. They get their name due to their resemblance to a kernel of corn. Corns are caused by repeated pressure on the skin, usually from shoes rubbing against the area. They can form on the soles of the feet, the tops of the toes, or in between the toes. Usually, the corns that form in between the toes are softer than those that form elsewhere on the foot. If you have corns that are causing pain or discomfort, a podiatrist can help treat them. The doctor may suggest changes to your footwear, prescribe orthotic inserts, or remove the thickened skin. For more information about corns on the feet, please speak with a podiatrist.
Corns are small, circular, thickened areas of skin on the feet that have a central core of hard material. They get their name due to their resemblance to a kernel of corn. Corns are caused by repeated pressure on the skin, usually from shoes rubbing against the area. They can form on the soles of the feet, the tops of the toes, or in between the toes. Usually, the corns that form in between the toes are softer than those that form elsewhere on the foot. If you have corns that are causing pain or discomfort, a podiatrist can help treat them. The doctor may suggest changes to your footwear, prescribe orthotic inserts, or remove the thickened skin. For more information about corns on the feet, please speak with a podiatrist.
Corns can make walking very painful and should be treated immediately. If you have questions regarding your feet and ankles, contact Dr. Todd Goldberg of Complete Family Foot Care Center. Our doctor will treat your foot and ankle needs.
Corns: What Are They? And How Do You Get Rid of Them?
Corns are thickened areas on the skin that can become painful. They are caused by excessive pressure and friction on the skin. Corns press into the deeper layers of the skin and are usually round in shape.
Ways to Prevent Corns
There are many ways to get rid of painful corns such as:
Treating Corns
Although most corns slowly disappear when the friction or pressure stops, this isn’t always the case. Consult with your podiatrist to determine the best treatment option for your case of corns.
If you have any questions please feel free to contact our office located in Littlestown, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
A corn is a lesion that forms in the skin of the foot, and it is typically circular in shape, small in size, and thick and rough in texture. A corn generally occurs as a result of repeated pressure on the skin; one example of this is the rubbing of a shoe against the skin. Corns differ from calluses in that their central cores are harder in texture.
A corn is a relatively common condition with a wide variety of treatment options. If a corn becomes overly uncomfortable or painful, consult with your podiatrist; he can determine the best method of treatment that is appropriate for you. Corns may return if the underlying cause of its development is not treated or removed. Avoid removing corns at home, as improper removal may cause infection.
A callus, similar to a corn, is an area of skin that has become thickened due to repeated pressure and rubbing. The rubbing causes the skin to create a layer of protective skin, which is the formed callus. Calluses can differ in size between people, and they can also become painful.
Multiple treatments are available for calluses. At-home treatment and removal should be avoided, as this can potentially lead to infection. Your podiatrist can best determine the cause of your calluses and suggest the treatment most appropriate for you.
 Warts that pop up on the bottom of the feet are known as plantar warts. One of many potential treatments for this condition is cryotherapy, in which the wart is frozen using liquid nitrogen. During this procedure, your doctor may first trim the wart. Sometimes, a local anesthetic may be injected into the area to reduce pain. Then, the doctor applies liquid nitrogen to the wart using a probe, cotton swab, or by spraying it directly onto the wart. Most warts require one to four cryotherapy treatments, with up to three weeks between treatments, to get full results. The area usually heals within one to two weeks with minimal or no scarring. If you suffer from plantar warts, it is suggested that you see a podiatrist to discuss treatment options.
Warts that pop up on the bottom of the feet are known as plantar warts. One of many potential treatments for this condition is cryotherapy, in which the wart is frozen using liquid nitrogen. During this procedure, your doctor may first trim the wart. Sometimes, a local anesthetic may be injected into the area to reduce pain. Then, the doctor applies liquid nitrogen to the wart using a probe, cotton swab, or by spraying it directly onto the wart. Most warts require one to four cryotherapy treatments, with up to three weeks between treatments, to get full results. The area usually heals within one to two weeks with minimal or no scarring. If you suffer from plantar warts, it is suggested that you see a podiatrist to discuss treatment options.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Todd Goldberg from Complete Family Foot Care Center. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
Treatment
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our office located in Littlestown, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar warts are described as small growths that appear on the heels or other areas of the feet that bear a large amount of weight. The pressure in these areas causes plantar warts to hide behind thick layers of skin called calluses. In most cases, plantar warts are not a serious health issue, and they usually go away without treatment. However, it is still important be mindful of them.
Plantar warts are caused by infections with human papillomavirus (HPV) in the outer layer of skin on the soles of the feet. The plantar warts then develop when the virus enters the body through weak spots at the bottom of the feet, such as tiny cuts and breaks. Plantar warts are not guaranteed for all who encounter the virus. Everyone responds differently to the affects of HPV.
Plantar warts are most common in the following groups: children and teenagers, people with weakened immune systems, people with history of plantar warts, and people who walk barefoot. Exposure to HPV is common in environments such as locker rooms or pool areas.
One of early signs to look out for is a callus, since many plantar warts hide behind them. You can also locate these warts by looking for small, fleshy, rough, grainy growths near the base of the toes and the heel. Early signs of plantar warts are shown by black pinpoints, which are small, clotted blood vessels. Lesions that interrupt normal lines and ridges in the skin of your foot may also be a sign of plantar warts. Any feeling of pain while walking or standing can also be a symptom of plantar warts.
Although most cases are not serious, some conditions may require a visit to your podiatrist. If you are uncertain that your lesion is a wart, if you have diabetes, or if you are experiencing bleeding, you may need to see a seek professional treatment. Your doctor may offer treatments such as prescribing stronger peeling medicine or using cryotherapy by applying liquid nitrogen to the wart. More serious cases may require minor surgery or laser treatment.
There are simple solutions available to help prevent plantar warts. One common task is to avoid walking barefoot in swimming pool areas and locker rooms, as this is where HPV is commonly present. Keeping your feet clean and dry, while changing shoes and socks daily can also help prevent future plantar warts. If you know someone who has plantar warts, it is important to avoid direct contact with their warts. You should also refrain from picking or scratching your wart if you happen to develop one.
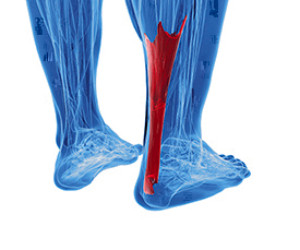 The Achilles tendon is the band located on the back of the leg and is responsible for connecting the calf to the heel bone. This tendon is responsible for allowing us to rise up on our toes and for us to push off when walking or running. There are 2 main types of injuries that can occur to the Achilles tendon. The first, known as Achilles tendinopathy, occurs when there are tiny tears in the tendon and around it, usually from overuse. The second injury, an Achilles tendon rupture, can cause sudden pain and loss of movement. This is usually caused by a sudden movement or force that stresses the calf muscle. Patients who are experiencing pain in their Achilles tendon should consult with a podiatrist because of the potential severity these injuries have. A podiatrist will examine the leg and determine the extent of the injury.
The Achilles tendon is the band located on the back of the leg and is responsible for connecting the calf to the heel bone. This tendon is responsible for allowing us to rise up on our toes and for us to push off when walking or running. There are 2 main types of injuries that can occur to the Achilles tendon. The first, known as Achilles tendinopathy, occurs when there are tiny tears in the tendon and around it, usually from overuse. The second injury, an Achilles tendon rupture, can cause sudden pain and loss of movement. This is usually caused by a sudden movement or force that stresses the calf muscle. Patients who are experiencing pain in their Achilles tendon should consult with a podiatrist because of the potential severity these injuries have. A podiatrist will examine the leg and determine the extent of the injury.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Todd Goldberg of Complete Family Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
Rupture Symptoms
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
If you have any questions please feel free to contact our office located in Littlestown, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
When you walk or run, the thick tissue on the bottom of your feet connecting the front of your foot with your heel—the plantar fascia—stretches and contracts. Repeated stretching and contracting of the plantar fascia can precipitate tearing or inflammation, otherwise known as plantar fasciitis. Runners are often afflicted with plantar fasciitis, which can cause a stabbing pain located on the bottom of the heel. Some simple at-home therapies for plantar fasciitis include refraining from activities that aggravate the area, icing it with an ice pack or massaging it by rolling a frozen water bottle under your feet. Additionally, a podiatrist may be able to help heal the plantar fascia by taping or splinting it, creating custom orthotics, or suggesting proper footwear and gentle stretching exercises.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Todd Goldberg from Complete Family Foot Care Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Littlestown, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
 Arthritis is a painful and debilitating disease that affects many millions of people in America. Rheumatoid Arthritis is one of the most common forms of arthritis and, in some cases, can begin as early as childhood. Rheumatoid Arthritis is an autoimmune disease where the joint lining is attacked by the body’s own white blood cells, triggering the lining to release harmful chemicals which ravage the joint’s surrounding bone, cartilage, and supporting tissues. This can occur in various joints—often on both sides of the body. People suffering with Rheumatoid Arthritis are encouraged to do what they can on their own such as: eating a healthy diet to manage their weight and stay healthy, doing modified exercises when they can, protecting their joints, and resting during flare-ups. If you are experiencing any joint pain, stiffness, or lack of mobility in your ankles or feet, it is suggested that you contact a podiatrist for relief of symptoms through a variety of treatments, medicines, and procedures.
Arthritis is a painful and debilitating disease that affects many millions of people in America. Rheumatoid Arthritis is one of the most common forms of arthritis and, in some cases, can begin as early as childhood. Rheumatoid Arthritis is an autoimmune disease where the joint lining is attacked by the body’s own white blood cells, triggering the lining to release harmful chemicals which ravage the joint’s surrounding bone, cartilage, and supporting tissues. This can occur in various joints—often on both sides of the body. People suffering with Rheumatoid Arthritis are encouraged to do what they can on their own such as: eating a healthy diet to manage their weight and stay healthy, doing modified exercises when they can, protecting their joints, and resting during flare-ups. If you are experiencing any joint pain, stiffness, or lack of mobility in your ankles or feet, it is suggested that you contact a podiatrist for relief of symptoms through a variety of treatments, medicines, and procedures.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Dr. Todd Goldberg of Complete Family Foot Care Center. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Littlestown, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.